|
If you are a professional or a writer who is passionate about health, racial, and social equity, consider contributing to our blog! Visit our Volunteer page to learn more. |
|
by Bree Bode, Karah Brink, Adriana Akers, Josh Leffingwell, Michelle Davis  Urban design is a critical concept for supporting the infrastructure and well-being of a city, catalyzing a higher quality of life, and optimizing equitable built environments (1,2). When constructs of urban design are paired with human design frameworks, approaches, practices, and principles, the potential to positively shift the social and political factors of health (SPFOH) in an equitable manner is more attainable (3,4). Without such frameworks, approaches, and inclusive practices, the concepts of urban design negatively impact people globally. When urban design has been paired with motives of xenophobia, racism, or gender bias, the comprehensive SPFOH have compromised livelihoods as seen in historical and recent examples in both the United States and Europe (5-7).
7 Comments
posted by Radhika Ramesh We hope you will be able to dedicate some time to relax and spend time with family and friends after a year of world-shifting events. Our team at Health Equity Initiative has been catching up on reading and listening these past few months, and these are examples of what we are reading or listening to on health, racial and social equity. Happy summer, and stay healthy and safe!
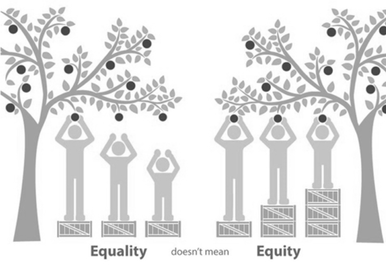
by Julia D. Day  Folkets Park in Copenhagen, Denmark Folkets Park in Copenhagen, Denmark If you're reading this blog, chances are you care deeply about achieving equitable outcomes. But how do you know if you're making progress? Working for health equity—defined as “all people having a fair and just opportunity to be as healthy as possible” (1)—is necessary, but how do we know when we have created environments that foster equity? And how do we ensure that terms like equity and inclusion aren’t just flimsy buzzwords, or worse, used to “equity-wash” something that isn’t equitable at all? To address these concerns, Gehl (an urban research and design consulting firm) teamed up with the Robert Wood Johnson Foundation (RWJF) and colleagues at the former Gehl Institute, to create the Inclusive Healthy Places Framework, which defines principles and metrics to guide and evaluate public space projects that support health equity (2). The Framework aims to demonstrate that public realm is a key component of health equity, and to create a platform through which more cross-sector partnerships can develop. by Sarah Carlson
One common form of implicit bias in health and social services is the differential treatment of male and female-presenting patients. Generally speaking, most people tend to make unconscious associations regarding masculinity and femininity, and these assumptions can impact the ways in which individuals understand and treat patients. In healthcare settings, widespread assumptions about men and women, such as the idea that men are more resilient and that women are more likely to express pain, might be detrimental and lead to inadequate treatment by healthcare professionals. As a result of such biases, patient needs can be overlooked (2).
by Alka Mansukhani , Lisa Goren and Renata Schiavo
Sadly, many students are not provided with an opportunity to learn about how their government works and may feel powerless about their ability to make an impact. Some may feel cynical and disconnected from public institutions and from centers of power. Educating students about local government, and modeling how to engage with those in authority would give them access and agency—both in local matters and in decisions affecting their lives. Most importantly, it would provide them with the skills they need to assess the impact of policies throughout their lives.
posted by Health Equity Initiative We are pleased to share this story on the importance of mutual aid during COVID-19 by Kaiser Health News, which was originally posted by our friends and colleagues at The Solutions Journalism Exchange. The story aligns with Health Equity Initiative's focus and advocacy efforts in support of community engagement and mobilization as a key strategy to advance health equity by raising the influence of community voices on intervention design and policy solutions. Mutual aid during the ongoing pandemic has emerged as a key action area to spread solidarity, build community, and help provide important services in our neighborhoods and cities that neither governments nor other organizations would be able to provide to the same extent without the input of community-specific groups and leaders. Enjoy and please share your own thoughts and experience on mutual aid during COVID-19 and beyond! Stay safe!  ‘It’s About Love and Solidarity’: Mutual Aid Unites NYC Neighbors Facing COVID By Elizabeth Lawrence, Kaiser Health News, July 27, 2020 NEW YORK CITY — Nancy Perez, a 45-year-old resident of the Brooklyn neighborhood of Bedford-Stuyvesant, contracted COVID-19 in March. She stayed quarantined in her room for a month to isolate from her two sons and grandson. A few days before she got the virus, she’d met a volunteer with Bed-Stuy Strong — one of the many mutual aid groups around the country that have rallied to provide help in the face of the pandemic. Bed-Stuy Strong assembled an army of volunteers to help vulnerable neighbors with food deliveries and basic supplies. While Perez was in isolation, volunteers regularly delivered cooked food for her sons, ages 17 and 20, and her 4-year-old grandson. Posted by Renata Schiavo, PhD, MA, CCL on behalf of all of us at Health Equity Initiative  All our hearts are broken by the pervasive racism and social discrimination that affect too many actions and policies in our society. We wish we had words that could provide meaningful comfort to the mix of outrage, pain, exhaustion, fear, or weariness many in our community are feeling in the wake of recent anti-black violence. We are not sure such words exist, but this we know for sure: We denounce the violence against the black community and stand in solidarity with all the families that have been affected by such violence. As an organization dedicated to advancing health equity and social justice, we cannot be silent as silence means complicity and directly contributes to trauma and to worsening health and social outcomes for black people. Our community stands together and is strengthened in its commitment to advancing health equity and racial equity. We have a difficult journey ahead of us…but we know that empathy, compassion and active anti-racism should inspire our commitment to justice and to promoting racial healing. As members of our community, we look forward to your ideas, so please share any suggestions we should take into account as we develop our action plan. We are committed to listen and to contribute to our collective work to address racism and social discrimination and transform our future. Please engage because #RacismIsAHealthEquityIssue and #BlackLivesMatter! Take good care everyone and stay safe. In solidarity from all of us at Health Equity Initiative. by Upal Basu Roy, PhD, MPH  It has been literally just about two months since I developed that fateful cough and slight breathlessness barely a month since COVID-19 had entered public health vocabulary. COVID-19 (short for Coronavirus disease-19) is caused by SARS-CoV-2, a type of virus that belongs to the same family of viruses that cause SARS (Severe Acute Respiratory Syndrome) and MERS (Middle East Respiratory Syndrome). The World Health Organization declared COVID-19 a global pandemic on March 11, 2020, reinforcing the contagiousness of this viral disease (1). As public health practitioners, we understand the severity of a viral pandemic that can have devastating consequences on the population. As of today, COVID-19 cases have been detected in all continents except Antarctica. I live in New York City, one of the first epicenters of the disease in the United States. One may automatically assume that NYC is adequately equipped to handle a pandemic the magnitude of COVID-19. I was incredibly lucky to have recuperated from COVID-19 without the need for hospitalization. But that does not stop me from reflecting on the glaring health disparities that COVID-19 has exposed in our community. While this is nothing new to public health practitioners such as myself, let us not underestimate the fact that COVID-19 has only amplified the many health inequities that already plague marginalized racial and ethnic communities in the United States. In other words, these inequities already existed! The pandemic merely exposed them. Communicating about Health Equity: Why Is There So Much Hesitancy among Communication Professionals?4/28/2020 by Chelsea Dade  “The single biggest problem in communication is the illusion that it has taken place,” said George Bernard. I’ve been thinking about the phrase that is circumventing our society, “stay safe at home.” While it’s used as advice to the general public, this term means different things to different people. What if you lack a home? What if you are in an abusive relationship? What if you cannot afford basic amenities to live? As communication professionals, we have to acknowledge that one common message cannot always translate, in words or in actions, for everyone. Just because a message is received, doesn't mean everyone can act upon that message. I’m a Health Communication Specialist who believes in the power of communication to improve health equity. But I’ve found that there is a great deal of hesitation when it comes to health communication professionals communicating about health equity. I’ve broken my hypothesis into three probable reasons. by Bree Bode and Friso van Reesema  Policy change has the ability to impact health and social outcomes during pandemics such as this unprecedented COVID-19 outbreak. As we know, the COVID-19 pandemic does not discriminate on the basis of geography or whether or not someone has a home where they can shelter-in-place. Rates of infection have been concerning both across urban and rural areas, including New York City and its suburbs, and rural areas in Louisiana, as well as international settings such as Lombardy, Italy. Reducing exposure to COVID-19 is critical to limit infections. As recommended by public health and medical experts, exposure to the virus can be reduced by closing schools, limiting operations of or closing non-essential services, staying home (if you have one) and practicing social distancing. In addition, fair public policies are essential for managing hospitals, COVID-19 testing, and the utilization of ventilators for patients in Intensive Care Units (ICUs). The Families First Coronavirus Response Act (FFCRA) includes an Employee Paid Sick Leave Rights provision. Yet, due to the economic disruption COVID-19 has caused, such a provision is insufficient to address ongoing financial insecurities faced by employees—whether they qualify or not for FFCRA benefits. In fact, the FFCRA and the related Paid Sick Leave legislation further expose a variety of health and social inequities that are concerning. Namely, FFCRA does not meet the needs of people who are historically and disproportionately impacted by poverty, which often goes hand in hand with low or no health insurance coverage (1,2). People who don’t qualify for FFCRA benefits and are also disproportionately impacted by poverty are likely to feel challenged by any potential decision of staying home, and reducing exposure, and instead may feel they should go to work, where unfortunately, their risk for contracting COVID-19 would increase. |
Archives
June 2023
CategoriesEditors:
Renata Schiavo, PhD, MA, CCL Alka Mansukhani, PhD, MS Radhika Ramesh, MA Guest posts are by invitation only. |



 RSS Feed
RSS Feed
